Researchers from the University of Pennsylvania investigated UK data covering over 1.5 million visits to doctors by 800,000 people with upper respiratory infections over a period of 20 years.
Just over 65% of the patients, who were all adults, received antibiotics for their infections. The patients were studied over 15 days following their first doctor visit to see how many were admitted to the hospital with pneumonia or any adverse event that might be related to the administration of the drugs, such as heart problems, liver or kidney toxicity, diarrhea and seizures.
Overall, there were 296 people admitted to the hospital with a case of pneumonia within 15 days of the initial doctor visit. That was 22 people admitted to a hospital with pneumonia for each 100,000 doctor visits if they did not receive an antibiotic – and 18 people per 100,000 who were treated with antibiotics.
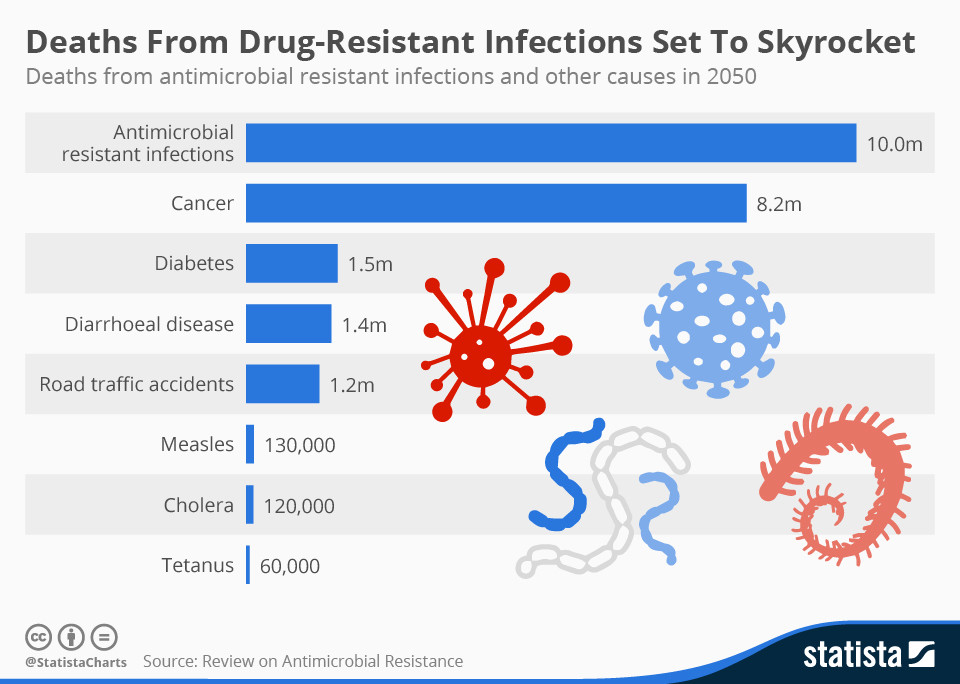
Researchers said that “12,255 or more people would have to be treated with antibiotics to prevent one person from being hospitalized.” We aren’t even talking about saving lives, just saving hospitalization. Considering the harm that antibiotics do to an individual’s gut health, and the rise of super bugs, it is immediately obvious that prescribing antibiotics for upper respiratory infections should be made illegal.
But no, we’ll keep on trusting that doctors know best.